April 4, 2016
Working Smarter and Sleeping Better: Circadian Rhythm in Workplace and Healthcare Design
As part of the Metropolis Think Tank series, Susan S. Szenasy visits the Seattle office of ZGF Architects LLP.
A project of ZGF Architects, The Federal Center South Building 1202 transformed a 4.6 acre brownfield site into a highly flexible, sustainable, and biophilic 209,000 SF regional headquarters for the U.S. Army Corps of Engineers (USACE) Northwest District.
Photo Courtesy ZGF Architects ©Benjamin Benschneider
On October 14, 2015, Susan S. Szenasy, Metropolis publisher and editor in chief, was in Seattle as part of the Metropolis Think Tank series to discuss both the need to consider circadian rhythm in workplace and hospital environments as well as the importance of understanding biophilia as a systems approach. What follows is an edited transcript of that conversation, prepared by Dora Vanette, with architects and designers at ZGF Architects LLP, their client, Seattle Children’s Hospital, and their colleagues and research partners at the U.S. General Services Administration (GSA) and the University of Washington. Think Tank 2016 is in full swing–early this June we’ll be in Washington DC.
CIRCADIAN RHYTHM IN THE WORKPLACE
SUSAN S. Szenasy, Metropolis (SSS): Knowing the architecture profession’s reliance on metrics and technology, I worry that these developments in the ways of 21st century design provide an excuse to create more tech solutions and less figuring out how a building really integrates with the natural environment. Can you convince me that I shouldn’t worry?
ED CLARK, Associate and Sustainable Designer at ZGF Architects LLP (EC): You don’t have to worry. Let’s start with something innately human, daylight. We see daylight as the primary or preferred light source. But we need to rely on electric light when daylight is not available, and the reliance on electric light and its consideration has evolved over time. Likewise, when the sustainable building discussion first began, the conversation considered buildings as machines first and places for human inhabitation second. Buildings were a technological means to an end: to reduce energy and water consumption. Today, we’ve gotten past that. It’s now poetic again to engage the natural world and provide low intensity design options in a way that is meaningful to inhabitants and to the overall human condition. In that same vein, we as a practice are re-engaging daylight with a renewed respect and an improved understanding of its effects on humans in a profound and meaningful way.
SSS: Still, I’m worried. Daylighting has become a mantra, which came with misunderstandings of what can happen when you create these incredibly luminous glass boxes. It’s very difficult to inhabit those buildings even when clad in high-performance glass. How do architects begin to use this system to create real relationships between us, the users of the building, and the natural world that we have evolved in?
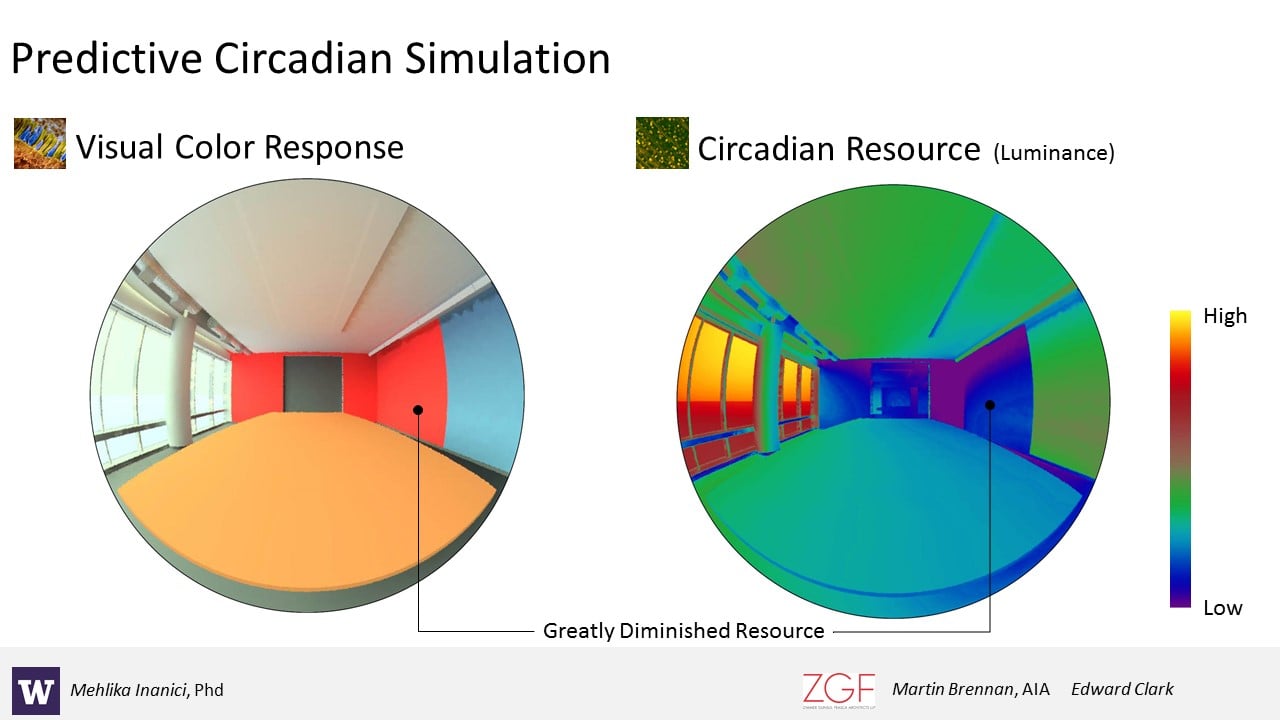
DR. MEHLIKA INANICI, Associate Professor, Department of Architecture, University of Washington (MI): There is a time when we need lighting to be able to perform a task, but there’s also a need for dynamism in lighting. Nature gives us that dynamism by default. But we seem to be increasingly more detached from nature, and we are lighting spaces as if we need the same level of lighting from morning to evening. Our research with ZGF is particularly aimed at creating tools that can be used in the design process—we’re not trying to push for more technology, but trying to use technology to support our connection to nature.
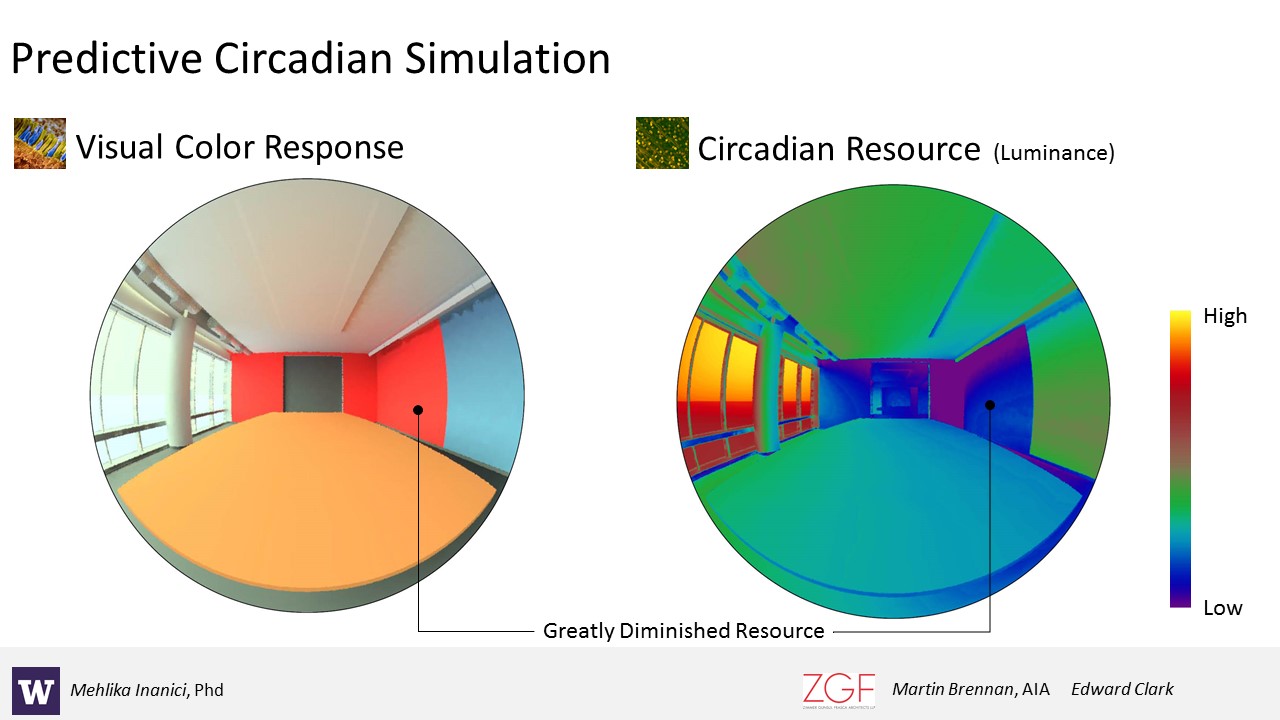
Collaborations between University of Washington and ZGF Architects produced the Lark Spectral Lighting project, an application (for grasshopper and rhino) to investigate circadian light metrics within a Radiance daylighting workflow. Lark includes tools to interpolate spectral data, build spectral materials, prepare spectral sky definitions and Radiance and DAYSIM methods to evaluate circadian illuminance and luminance.
Image Courtesy ZGF Architects
DR. JUDITH HEERWAGEN, Program Expert, U.S. General Services Administration, Office of Federal High Performance Green Buildings (JH): In one project, we monitored how much light exposure office workers naturally get. We found that people near the windows did pretty well, but the more you got into the interior, the more you experience biological darkness for much of the day. We found that those folks have poorer sleep, and they’re sleepy during the day. We know we can’t get daylight to everybody all the time, so how do we begin to integrate it with what we’re learning? How do we integrate lighting with design—and not just lighting, but the colors we use, ways we design interior spaces, and create decisions on who gets to be near the windows and who doesn’t? We came up with some novel ideas such as having a light oasis or some place that people could go to get some light. Our challenge is to do this in an energy effective way. I worry that we’re going to push too much in the direction of technology because it’s an easier solution than dealing with light coming in through the windows. So one of the projects we’re working on with Rensselaer Polytechnic Institute and ZGF is looking at a film we can put on windows to bounce light further into spaces. Yes, we’re looking at technology solutions, including those that allow designers to analyze the circadian light source, but we want to do everything in the least expensive, most effective, and most energy efficient way.
CIRCADIAN RHYTHM IN HOSPITALS
SUSAN GEIDUSCHEK, Senior Director & Associate Chief Nurse at Seattle Children’s Hospital (SG): The goal with enforcing circadian rhythm is to help patients achieve a sense of normalcy. In some intensive care areas, for instance, patients get confused as to when it’s day and when it’s night, so the quicker we can correct that challenge, the sooner the patients can return to their normal rhythms.
What we want when we design a successful building is an exceptional experience for patients—one that would promote healing and normalcy—but we also want an exceptional experience for the staff. For instance, at night we don’t want our nighttime workers to go to sleep, but we want our families to sleep, and I think that’s our next operational challenge—how do you integrate both of these different rhythms? I agree that cost and high tech can sometimes be problematic. Our staff and our families don’t know how to manage this technology, so we have to keep it simple in order to cut operational costs and the training of staff and families.
SSS: Nurses are there to help us, but they’re not being helped to live healthy lives because of the rigors of keeping everything on track, because of the systems in the hospital that keep overworking them.
SG: As part of our design process at Seattle Children’s Hospital, we were charged with some key requirements on safety and efficiency. One of our targets was to decrease travel distances, both for the family and the staff. For instance, the distance for a nurse to walk from a patient’s room in our oncology unit to the medication room was 180 feet. The oncology unit has a lot of medications, and for safety reasons nurses could only get one medication a time, so they would have to walk back and forth. All that time walking is inefficient. It doesn’t allow nurses to be at the bedside—where they want to be and where the patients want and need them to be. We tested various designs, and one of the things we did was decentralize medication storage and delivery to the room.
The other issue was search time. The nurse spends a lot of time searching for different people and sources of information. That’s a waste in their workflows as well, so we designed a shared unit where we wanted the physicians to be as well, so the nurses aren’t searching for them all the time. The theory was that if they shared workspaces and were centrally located doing their work together, we would actually advance care and see that as a decreased length of stay for the patients. That has also proven to be effective. We’ve seen significant improvement in different outcomes.
Another one of our baselines was how much time a nurse actually spends in a patient’s room during a shift. We started at 26 percent and moved that to 76 percent. We thought about what drives a nurse to stay in the room and how that supports healing. It’s an easy concept to get people to understand—nurses want to be at the bedside, they don’t want to be tracking people down and looking for information. I think, on the whole, we are seeing some nice changes in how design facilitates nurse workflow.
SSS: What’s interesting about these projects is that they strive for efficiency, but efficiency from the human point of view. That’s a huge turn of attitude; it’s bound to improve everybody’s life for the better in healing environments.
LISA REITZES, Project Manager, Facility, Design & Construction Department, Seattle Children’s Hospital (LR): I’m part of a working group at Seattle Children’s with a goal to articulate and prioritize our commitments to healing environments. The art program we have developed creates a calming and healing experience, whether you’re in the public spaces or in the patient units. It provides a sense of quiet but also a way to stimulate the imagination, ways to tell stories, to pull people out of the place where they are—dealing with really hard healthcare situations—and create images and places that are memorable, that tap into memories of natural environments that the patients have known.
I know landscape imagery isn’t necessarily the same as having windows, but it can create a psychological pathway through the imagination. These paintings help people inhabit a sense of space, even if they can’t have it—they can create a view out.
CONNECTING INSIDE AND OUTSIDE
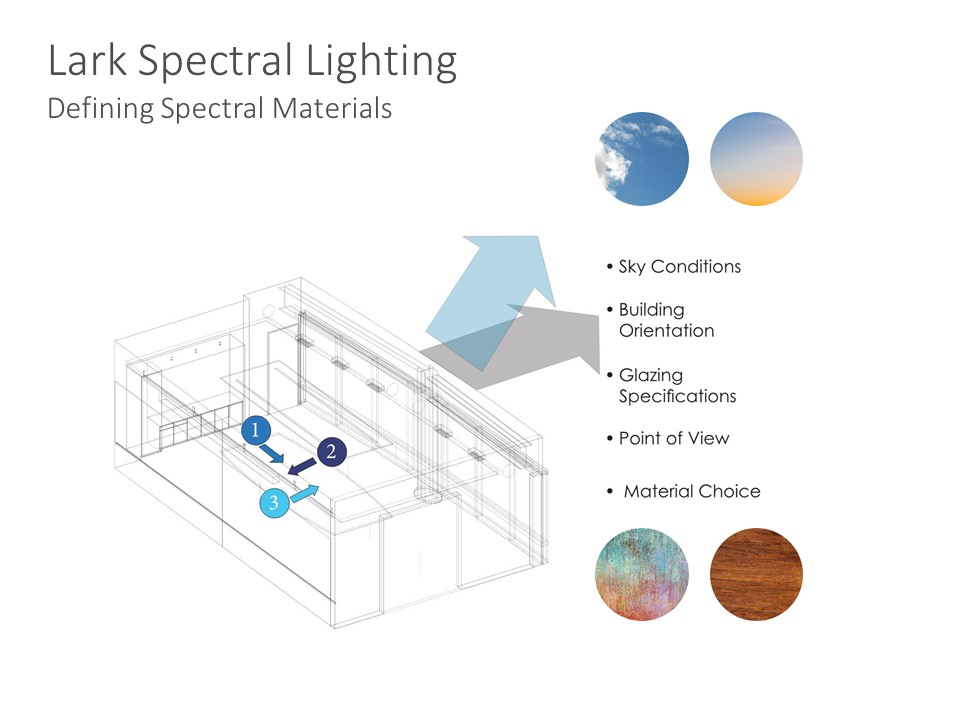
As part of the process of using the Lark Spectral Lighting application, users must define spectral materials. The app will then allow them to interpolate spectral data and evaluate circadian illuminance and luminance
Image Courtesy ZGF Architects
SSS: What is the current thinking about circulating air from the outside at certain times or ways of cleaning out the mechanical air that everybody’s breathing in hospitals? Designers working on hospitals could be doing really good work with operable windows, with bringing in the sunlight, with creating a much more humane and biophilic environment.
JH: Certainly people like fresh air, and the sense of air movement on our bodies, and if you have places, such as roof gardens in the hospitals, that is a great idea. How many of you would like to live in a house where you could not open the windows, so why do we do it in hospitals and workplaces? This is a huge part of biophilia.
SSS: What you said is so important to us, especially because designers have been using the word biophilia without really understanding what it means. It is much more complex than putting a plant on a table, or a painting of nature on the wall.
JH: Biophilia is not merely decoration. But we’re using it now as a decoration. Biophilia is a system of design that includes air, touch, our whole sensory system. There’s something about our sensory systems that’s so connected to nature. And we haven’t talked about sounds. How about sounds in a hospital? Bleep, bleep, bleep all night long. One of the big stressors in a hospital is the noise. We have yet to explore the biophilia of sound, the biophilia of touch. But I think that once designers start thinking about it, then you’ll begin to see biophilia as a design system. But we’ll need to remember that there are things that we need to avoid. Nature is not always good. We need to understand what and how to avoid things that are harmful. I think if we look at biophilia as a system, we wouldn’t think of it as a painting you put on the wall, a plant you bring in; it’s a totally different way of thinking about design.
Everyone, designers particularly, have to learn how to have a conversation with a client, where they talk about life processes that are part of the whole system. Biophilia should be intuitive because it is part of our genetic make up. The notion of refuge is essential to our human experience; you want to be in a place where you can see out. You feel really uncomfortable when you can’t be seen by others and you can’t see them.

Panelists at the ZGF Architects Think Tank in Seattle– from left to right: Ed Clark, Susan S. Szenasy, Lisa Reitzes, Judith Heerwagen, Susan Geiduschek, Dr. Mehlika Inanici, Kari Thorsen, Mark Gesinger
Photo Courtesy ZGF Architects
MATERIAL SOURCES
SSS: Let’s talk about materials. So many of our materials are composed of things we don’t know much about, or that that we know are carcinogenic. So how do we start that conversation about materials, especially in a hospital environment where health is the primary concern—and hospital design can set the goals for the rest of society.
KARI THORSEN, Associate Partner and Interior Designer, ZGF Architects LLP (KT): It’s really hard. Vinyl is a great example. All of our healthcare clients want to use vinyl because it’s the only thing that can be used with the harsh chemicals they’re using.
One thing that we do at ZGF, we push our manufacturers to declare the Red List chemicals in their products. We also tell our clients that they need to clean these materials differently. When you use 50 percent bleach and water and not wipe it down afterwards, the material will break down. It’s a constant education process. We can push the manufacturers, say we’re not going to specify your products if they contain chemicals from the Red List, but we first need to know what’s in their products.
EC: We’ve been working with our peers in practice, creating a network of champions we find within other firms. But it’s an overwhelming conversation with many players and an exorbitant amount of information. And at some point you understand that a lot of the chemistry in the products available for us to specify is proprietary, that manufacturers believe that they can’t share the information because sharing is perceived as a market risk.
We, as an industry, have stored away hundreds of spreadsheets of egregious chemicals, but no one wants to look at a spreadsheet in the end. So the question remains, how do you make this information digestible and informative in a very efficient manner? That’s where we are with materials today. It’s a terribly difficult problem. But it’s not unsolvable, and the more pressure the collective (practitioners, owners, building occupants) puts on manufacturers to be transparent and provide healthier options, the more they’re going to respond to market demand.
JH: The problem has to be solved through pressure on the chemical industry. Yes, we all benefit from some of the chemistry. The industry creates things that make our lives easier and better. But we have come to rely on chemistry too much.
Throughout human history, we’ve gone from really hot to really cold, we’ve had natural ways to deal with regulating temperature. Now we’re used to mechanical and chemical ways. This is going to be a huge problem to solve. We’ve got really serious problems in the future with climate change—we’re not going to be comfortable, we’re going to be discomforted. The question is how we deal with that.
The Metropolis Think Tank series is presented in partnership with our sponsors, Bretford, DuPont Solid Surfaces, Sunbrella, and USG.
Ed Clark, Associate and Sustainable Designer and Kari Thorsen, Associate Partner and Interior Designer, ZGF Architects LLP. Dr. Judith Heerwagen, Program Expert, U.S. General Services Administration, Office of Federal High Performance Green Buildings (GSA); Dr. Mehlika Inanici, Associate Professor, Department of Architecture, University of Washington; Susan Geiduschek, Senior Director & Associate Chief Nurse at Seattle Children’s Hospital; Lisa Reitzes, Project Manager, Facility, Design & Construction Department, Seattle Children’s Hospital; Susan S. Szenasy, Metropolis.





