February 1, 2013
How MASS Design Group Applies Developing-World Lessons to U.S. Hospitals
MASS Design Group takes the health-care lessons learned in the developing world to regulation-bound U.S. hospitals.
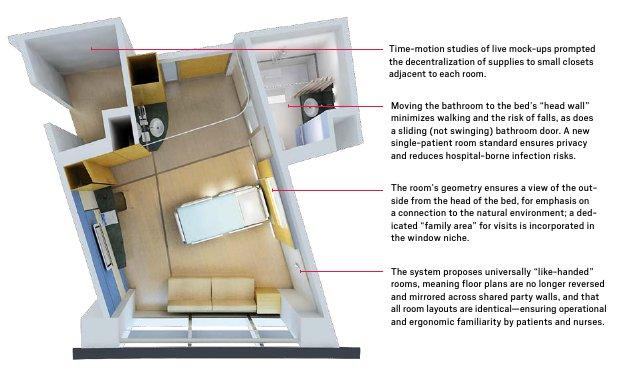
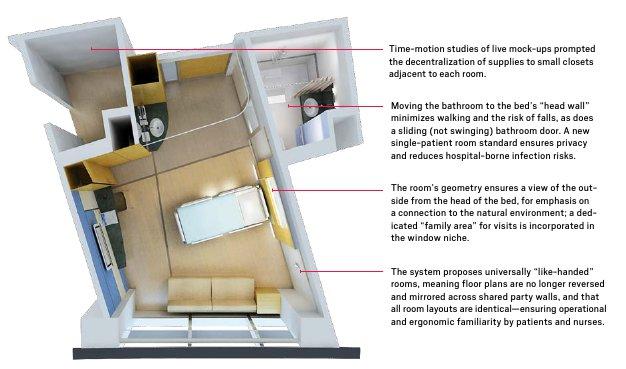
Room of the Future
MASS’s 2012 Hospital of the Future project deployed a state-of-the-art “baseline room” based on a prototype for a New Jersey hospital, developed by collaborator Rosalyn Cama and architects from HOK.
Courtesy CAMA
It was a really great example of a perfect failure.” That’s how Michael Murphy, executive director and co-founder of the Boston-based MASS Design Group, recalls a presentation he gave last year at an upstate New York hospital. The hospital had invited MASS, along with New Haven health-care interior design firm CAMA, to see how their experience designing health-care facilities in developing countries like Rwanda and Haiti could be applied to envisioning a Hospital of the Future—and how that vision could be developed from an existing facility. The failure Murphy cites wasn’t in his presentation, but in that facility: “It was a warm day in May,” he recalls, “and it was already getting hot, and the building’s air conditioning had shut down, and during the meeting the temperature in the room was slowly getting up to around 100 degrees, with a really high dew point. We went to open the windows, and they were literally bolted shut.”
Among the features Murphy was proposing that day were, of course, operable windows. Ironically, he says, “the hospital was a relatively innovative Brutalist design from the 1970s, and already had these beautiful double-layered windows with a center swivel, which could open almost fully for maintenance or airflow regulation, with dust-free blinds integrated between the glass panels”—exactly the kind of feature he would have recommended. Except for the bolts, which most likely reflected post-occupancy security concerns and decisions to exclusively regulate temperature and humidity with mechanical systems. Local adjustability, of everything from windows to furnishings, was a major theme in the MASS/CAMA presentation, a reversal of a decades-long tendency toward centralization and standardization of facility systems and components in large-scale institutional buildings—especially hospitals.
The MASS/CAMA proposal essentially turned the edifice’s entire facade into an operable window by removing the hospital’s precast concrete wall panels and replacing them with a lightweight, multilayered system with localized customizations including daylighting, airflow, and other variables. Removing the structural load of those heavy panels also meant that the existing building could eventually accommodate additional floors without being reinforced. “Instead of demolishing,” Murphy says, “we looked at how to use what’s already in place, so we rethought the surface as a mechanism for performance, with a deep double-skin system,” incorporating shading, outdoor balconies, and a three-foot gap between interior and exterior glass, along with “vertical solar chimneys to accelerate the extraction of air and pull fresh air into public areas of the interior—a filtration system more like natural breathing.”
Those solar chimneys, which use the natural rising of sun-heated air to aerate a building without mechanical systems or electrical power, were a detail MASS first encountered in southern Rwanda. The Hospital of the Future project is an example of what Murphy calls “South-to-North thinking,” in which robust and adaptive design solutions developed under the sometimes-extreme conditions of the developing world can be applied closer to home. The MASS group itself followed a special trajectory along that axis: in 2006, when Murphy and Alan Ricks (MASS cofounder and COO) were still studying architecture at Harvard’s Graduate School of Design, Murphy connected with Dr. Paul Farmer, the cofounder of Partners in Health (PIH), a global advocacy group, and with the Rwanda Ministry of Health—and then found himself, right out of school, in an intense collaboration with local artisans and physicians in the yearlong design-build of the innovative Butaro Hospital. That project, an elegantly Aalto-esque compound on the hillside site of a former military base in the Burera district, became the first in a constellation of high-design, low-cost, health- care, education, and housing projects MASS has participated in developing across central and west Africa.

The low orange headwall along the center of MASS’s Butaro Hospital wards ensures that beds face out toward daylight and views of nature. Running electrical and technical services through the low wall means they can be maintained and updated easily.
The guiding principles of the Butaro project included what Ricks described as, “not designing a perfect building, but a building that is capable of failing safely, with passive systems always supplementing mechanical systems, always coming back to an idea of resilience—which of course is the hot topic right now,” in our era of economic scarcity and increasingly extreme weather. At Butaro, this approach included such seemingly simple moves as eliminating hallways and moving building circulation into perimeter verandas to reduce airborne pathogen transmission, and concentrating technical systems like pipes, conduits, and monitors into a low half-height wall along the center of each ward, meaning that beds could face outward from that wall to receive daylight and views, and that those systems can be frequently serviced and modified without significant disruption to daily operations.
While the architecture of health care in the United States doesn’t face the acute crises of places like Rwanda, it is nevertheless in trouble. Roger Call, the incoming president of the American Institute of Architects Academy of Architecture for Health (AIA/AAH), a 6,000-member specialty group, acknowledges that members of the industry have made some mistakes as a profession in handling health-care design, but emphasizes the complexity of the problem: “You have tech-heavy environments, you have highly regulated, code-intensive environments that you have to survey and certify regularly, with an exponential growth of information and knowledge management in both design and operations.” With the passage of the Affordable Care Act, an aging American population, and a shifting emphasis toward ambulatory care over traditional hospital stays, Call foresees a growing demand and stretched resources. “The expectation for outcomes is going to be higher,” he says, “and there’s a need to apply a continuous improvement [to architectural design].”
In the U.S., Murphy observes, hospitals are subject to “incrementally implemented and overlapping zoning codes, which can make it difficult in some cases to innovate. And many existing buildings suffer from the same kind of implementation problem, in which buildings are aggregated over time. Most hospital buildings were intended to grow and accommodate change in a systematic way, but they get stuck, fixed in time, or sprawl horizontally. The result is a maze-and-labyrinth problem. By trying to create a highly controlled interior, you get superblock buildings that perform very poorly.” Similarly, hospital environments also often feature overlapping palimpsests of built-in technological systems in which the state-of-the-art and the semi-obsolete have to contend with each other. Innovation can be easier when you’re starting from scratch. “When there are no existing structures, it’s obviously problematic for the local population, but it also means we can leapfrog legacy systems,” Ricks says, comparing that leap with how online mobile banking has rapidly become the norm in central Africa, bypassing brick-and-mortar storefronts altogether. Rwanda, Murphy notes, faces severe limitations in its health care infrastructure, but neither is it “burdened by a stifling system of codes and regulations,” which, however necessary and well-intentioned, can strangle creativity.
These kinds of challenges arose during a recent project MASS undertook to study the development of a pediatric cerebral palsy center at a Cincinnati-area hospital. While the requirements of the Americans with Disabilities Act (ADA) generally ease access and ergonomics for all building users, MASS suggested an even more specialized customization of the center’s architectural environment and furnishings. “Even those ADA codes were not meeting the needs of severely mobility-impaired patients,” Murphy says. And sometimes they require modifications to enable environments at the right scale, and with the right features, for the children the center serves. “We have to expand the problem somewhat, and at the same time focus tightly case-by-case,” Ricks says. “It’s not just about building, but rethinking accessibility and whether certain codes are serving specific patients, and serving all the mechanisms in place for them in the architecture.”
And yet, among the factors determining health-care outcomes, architecture often ends up low on the list—even though it has a critical impact, from concrete issues like limiting hospital-acquired infection rates, to more abstract missions like establishing connections to the natural environment. “Clinicians aren’t always accustomed to thinking of design as a factor in positive outcomes,” Call says. “I say this as the husband of a nurse: clinicians have a great attitude of just dealing with what they have, so they take the architectural space as a given. They are great users of Scotch tape to adjust their environments, to create workarounds, and just get on with the job.” While that approach represents a kind of operational resilience equivalent to the architectural resilience MASS developed at Butaro, it often results in dispiriting, even dysfunctional, interiors. “So often at a hospital,” Call says, “I walk into a beautiful lobby and then the exam room looks like a utility closet. And the rooms mishandle simple things like daylighting and acoustics, so they aren’t even places you’d want to sleep, let alone recover from illness.”
Ironically, it’s exactly the kind of vigilant evidence-based experimentation that clinicians apply in diagnosis and treatment that may enable designers and engineers to fix those basic architectural problems. The single-patient room that MASS, in collaboration with CAMA, applied to its Hospital of the Future project grew out of a “baseline room” that CAMA principal Rosalyn Cama developed with architects at HOK for the new campus of the Universal Medical Center of Princeton at Plainsboro, New Jersey (UCMPP), which opened last May. “For that room,” Cama says, “we actually built a live mock-up on an existing hospital floor, and the data we got from watching how it was used, and the tweaking we were able to do, was invaluable in establishing this new baseline room, which became probably the most advanced design at the time.”
“The problem with health-care design,” Cama says, “is you have designers intimidated by the fact that they are accommodating medical procedures, so they ask the doctors the wrong question: ‘What do you want?’ The doctor does a mental inventory of their existing environment, fixing each thing about it, and what happens is that the architect designs a better old hospital, instead of a new one.” Because MASS “has studied how to solve problems with such limited resources, and knows how to solve them simply,” Cama says, the architects were well-equipped to break that cycle. “Having looked at the logic behind those simple solutions they come back here and ask, ‘Okay, what are our materials, what are our possibilities?’” she says, adding that when she was looking at architects to partner with on the Hospital of the Future project, “I knew what all the other firms would do, but I had no idea where it would go with MASS, and I thought that would be awesome.”
MASS and CAMA developed their project in a short seven-week sprint last spring. Roger Call, in his role as director of health care architecture and design for Herman Miller Healthcare, recently partnered with MASS for an even more intense one-week design project to develop custom beds and chairs for the Gheskio Clinic in Haiti, which has been addressing the cholera epidemic that followed the 2010 earthquake there. The result, plastic tensile structures on interlocked butterfly-like supports, happens to be beautiful. But more important for Call is that it is, “economical, durable, deployable, repairable, and interchangeable.” And that it had such a rapid turnaround time. “The parallel I see,” Call says, “is to the application of the Herman Miller Performance System,” a lean manufacturing strategy adopted from Toyota operations management in 1995. That system replaces centralized and routinized fabrication, warehousing, and distribution methods with on-demand, small-batch, rapid-turnover production cycles that result in a more nimble company.” Applying this kind of system to design and construction,” Call says, “would be a big deal in health care. The goal is not to design the perfect clinic, but to design a space that can adapt to change quickly, easily, and daily. The conversation between operational design and physical plant design has got to be much closer.” This conversation starts, for Call, with a motto he attributes to legendary engineer Shigeo Shingo, who developed the Toyota Production System in the 1970s. It’s a conclusion that would have been familiar to MASS’s Michael Murphy on a hot day last May: “Bolts,” Shingo said, “are the enemy.”





